Are you tired of the constant discomfort and unpredictable nature of irritable bowel syndrome (IBS)? If so, you’re not alone. IBS affects millions of women worldwide, causing a range of symptoms that can significantly impact their daily lives. But fret not, because we’re here to provide you with insightful information and effective tips to manage those bothersome IBS flare ups.
As an Ayurvedic doctor with over 40 years experience in holistic natural healing, I have seen and treated countless patients, who were suffering from chronic IBS symptoms. Along with, our team of experts at Medhya Herbals has meticulously researched the subject, thus bringing you the most reliable information to regain control over your gut health.
In this comprehensive article, I will delve into the world of IBS flare ups, exploring the symptoms, triggers, and effective treatment options. Whether you’re seeking relief from abdominal pain, bloating, or unpredictable bowel movements, I have you covered.
By the end of this article, you’ll gain a deeper understanding of what IBS flare ups truly feel like, how to identify potential triggers, and most importantly, effective strategies to soothe and manage those flare ups naturally. I’ll guide you step-by-step, providing practical advice on the best foods to eat, lifestyle adjustments to make, and the role of Ayurveda in promoting a healthier gut.
So, if you’re ready to take charge of your IBS and experience a life with fewer flare ups, read on! Our insights and expertise will empower you to make informed decisions about your well-being, giving you the relief and freedom you deserve. Say goodbye to the frustration and discomfort of IBS and embrace a life of balance and wellness.
Understanding Irritable Bowel Syndrome – IBS Flare Up
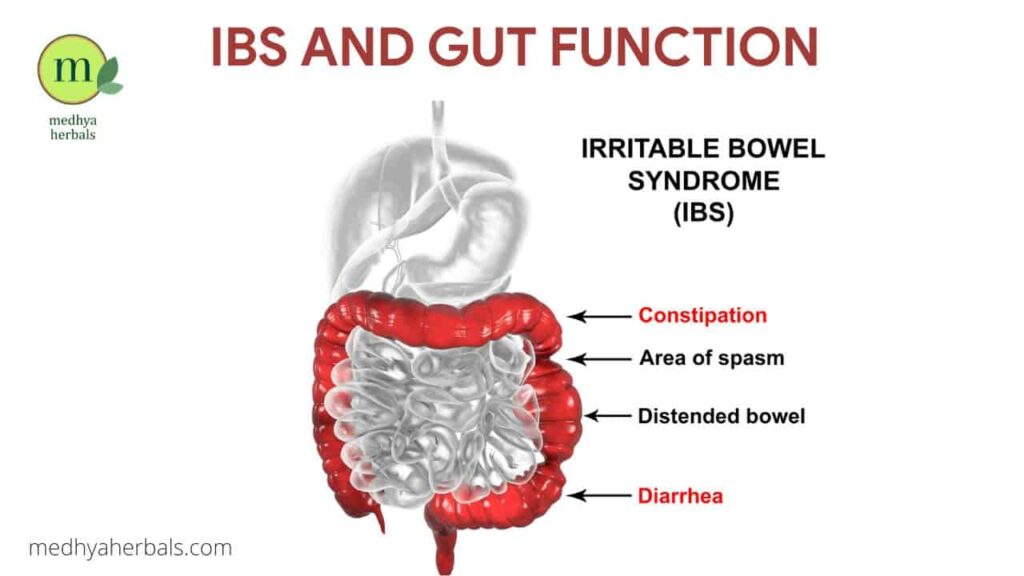
IBS, or Irritable Bowel Syndrome, is a chronic gastrointestinal disorder that affects the large intestine (colon). It is characterized by a combination of various symptoms, including abdominal pain, bloating, changes in bowel movements (such as diarrhea, constipation, or both), and an overall sense of discomfort.
During an IBS flare up, the symptoms of the condition intensify, causing increased discomfort and disruption to daily life. An IBS flare up can feel incredibly distressing and disruptive. It may leave you feeling helpless and frustrated.
How Long does IBS Flare Up Last?
The duration of an IBS flare up can vary from a few hours to several days or even weeks. Factors that influence the length of a flare up include:
- Individual Differences: Each person’s IBS symptoms and flare ups can vary in duration and intensity.
- Trigger Factors: The presence of specific trigger factors, such as stress, certain foods, hormonal changes, or infections, can influence the length of a flare up.
- Treatment and Management: The effectiveness of management strategies, including dietary modifications, lifestyle changes, and medication, can play a role in shortening the duration of an IBS flare up.
IBS Flare Up Symptoms
The specific symptoms experienced during a flare up can vary from person to person. Some of the common sensations experienced during an IBS flare up include:

Abdominal Pain and Cramping
Increased pain and discomfort in the abdomen.
- Intense or sharp pain in the abdomen, often concentrated in the lower abdominal area.
- Cramping sensations that can range from mild to severe, with spasms and waves of pain.
Bloating and Distension
Heightened bloating, making it difficult to fit into clothes comfortably.
- Abdominal bloating, where the belly feels swollen or larger than usual.
- A sense of fullness or tightness in the abdomen.
Altered Bowel Movements
Unpredictable changes in bowel habits, leading to anxiety and embarrassment.
- Diarrhea: Frequent loose or watery stools that may be urgent and difficult to control.
- Constipation: Infrequent bowel movements characterized by difficulty passing stools and straining.
Changes in Stool Consistency and Appearance
A sense of fatigue and low energy due to disrupted sleep patterns and the physical toll of flare ups.
- Stool may appear different during an IBS flare up, such as looser or harder than usual.
- Mucus in the stool, which may be more noticeable during flare ups.
What Triggers IBS Flare Ups?
IBS flare ups can be triggered by various factors, and identifying these triggers is crucial in managing the condition effectively. While the exact cause of IBS is not fully understood, some common triggers include:
1. Food Sensitivities
Diet plays a significant role in triggering IBS flare ups. While triggers can vary from person to person, there are common dietary factors that may contribute to symptoms. Here are some ways certain foods can trigger IBS flare ups:
FODMAPs
FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) are a group of carbohydrates that are poorly absorbed in the small intestine. They can ferment in the colon, leading to gas, bloating, and diarrhea in some individuals with IBS. Common high-FODMAP foods include wheat, onions, garlic, dairy products, apples, and watermelon.
Trigger Foods
Certain foods may directly irritate the gastrointestinal tract or stimulate the nerves in the gut, causing symptoms to flare up. Common trigger foods for IBS include spicy foods, fatty foods, caffeine, alcohol, and artificial sweeteners. However, trigger foods can vary from person to person, so it’s important to identify individual triggers through a food diary or elimination diet.
2. Stress and Emotional Factors
Stress and emotional factors play a significant role in triggering IBS flare ups. Emotional distress, anxiety, and depression can exacerbate symptoms and contribute to the onset of flare ups.
3. Hormonal Changes
Hormonal fluctuations, particularly in women, can influence the occurrence and severity of IBS symptoms. Many women report an increase in symptoms during menstruation.
4. Medications and Antibiotics
Certain medications, such as antibiotics, can disrupt the natural balance of gut bacteria, leading to IBS symptoms and flare ups. It is important to discuss potential side effects with your healthcare provider.
5. Gut-Brain Axis Dysregulation
The gut-brain axis refers to the bidirectional communication between the brain and the gut. Disruptions in this connection can contribute to IBS symptoms. Factors that affect gut-brain axis regulation, such as abnormal serotonin levels or altered gut motility, may trigger flare ups.
How to Identify the IBS Triggers?
Identifying individual IBS triggers can be a process of trial and error. It involves closely monitoring your symptoms and identifying patterns. Here are some steps to help determine your personal triggers:
- Keep a Symptom Diary: Record your daily food intake, stress levels, medication use, and any other factors that may influence your symptoms. Note the occurrence and severity of IBS symptoms during flare ups.
- Elimination Diet: Consider following an elimination diet under the guidance of a healthcare professional. This involves temporarily removing common trigger foods, such as FODMAPs, and gradually reintroducing them to observe their effects on symptoms.
- Professional Guidance: Consult with a healthcare provider, such as an Ayurvedic doctor or a gastroenterologist, who specializes in IBS management. They can provide guidance, conduct tests if necessary, and help identify specific triggers based on your unique situation.
IBS Flare Up Treatment
When it comes to treating an IBS flare up, there are various approaches, including conventional and Ayurvedic treatments. Both aim to alleviate symptoms and improve overall well-being. It is important to consult with your healthcare provider to determine the most suitable treatment plan for your specific needs.
Conventional Treatments
Conventional treatments for IBS flare ups may include:
- Dietary Modifications: Working with a registered dietitian to identify trigger foods and create a personalized diet plan that suits your needs.
- Medications: Your healthcare provider may prescribe medications such as antispasmodics, antidiarrheals, laxatives, or low-dose tricyclic antidepressants to manage specific symptoms.
- Psychological Support: Cognitive-behavioral therapy (CBT), relaxation techniques, and stress management strategies can help alleviate anxiety and manage stress-related IBS symptoms.
Ayurvedic Treatments
Ayurveda, an Indian holistic medicine system, offers natural remedies to manage IBS flare ups. Ayurvedic treatments focus on restoring balance to the body and promoting overall well-being. Some Ayurvedic approaches for IBS management include:
- Herbal Supplements: Ayurvedic herbs like triphala, licorice, and peppermint may be used to help soothe the digestive system and reduce IBS symptoms.
- Diet and Lifestyle Modifications: Ayurveda emphasizes dietary changes tailored to an individual’s dosha (unique mind-body constitution). Lifestyle adjustments such as regular exercise, stress reduction techniques like yoga and meditation, and adequate sleep can also be beneficial.
- Panchakarma: In severe cases, Ayurvedic treatments like panchakarma, which involves detoxification therapies, may be recommended to restore balance and promote digestive health.
Ayurvedic Herbal Supplements for IBS Flare Up Treatment
Ayurveda offers a range of herbal remedies that may help manage IBS flare ups. It’s important to consult with an Ayurvedic practitioner or healthcare professional before starting any herbal remedies to ensure they are suitable for your individual needs. Here are some Ayurvedic herbal remedies commonly used for IBS flare ups:
- Triphala: Triphala is a blend of three fruits (amalaki, bibhitaki, and haritaki) known for their digestive properties. It helps regulate bowel movements, relieve constipation, and support overall digestive health.
- Licorice (Yashtimadhu): Licorice has anti-inflammatory and soothing properties that can help reduce inflammation in the gastrointestinal tract and alleviate symptoms of IBS.
- Peppermint (Pudina): Peppermint is commonly used to ease digestive discomfort and relieve abdominal pain and cramping associated with IBS.
- Fennel (Saunf): Fennel seeds have carminative properties that help reduce bloating, gas, and abdominal discomfort.
- Ginger (Adrak): Ginger is known for its anti-inflammatory and digestive properties. It can help reduce inflammation in the gut and relieve symptoms such as nausea, bloating, and abdominal pain.
- Brahmi (Gotu Kola): Brahmi is an herb that is known for its calming and stress-reducing effects. It can help alleviate stress-related IBS symptoms and promote overall well-being.
- Shankhpushpi: Shankhpushpi is an herb that helps calm the nervous system and reduce anxiety, which can contribute to IBS symptoms.
- Aloe Vera: Aloe vera has soothing and anti-inflammatory properties that may help reduce inflammation in the gastrointestinal tract and relieve symptoms of IBS.
Natural Home Remedies to Soothe an IBS Flare Up
When experiencing an IBS flare up, there are several strategies you can try to help soothe and calm your symptoms. It is important to note that what works for one person may not work for another, so it’s essential to find what works best for you. Here are some general approaches to consider:
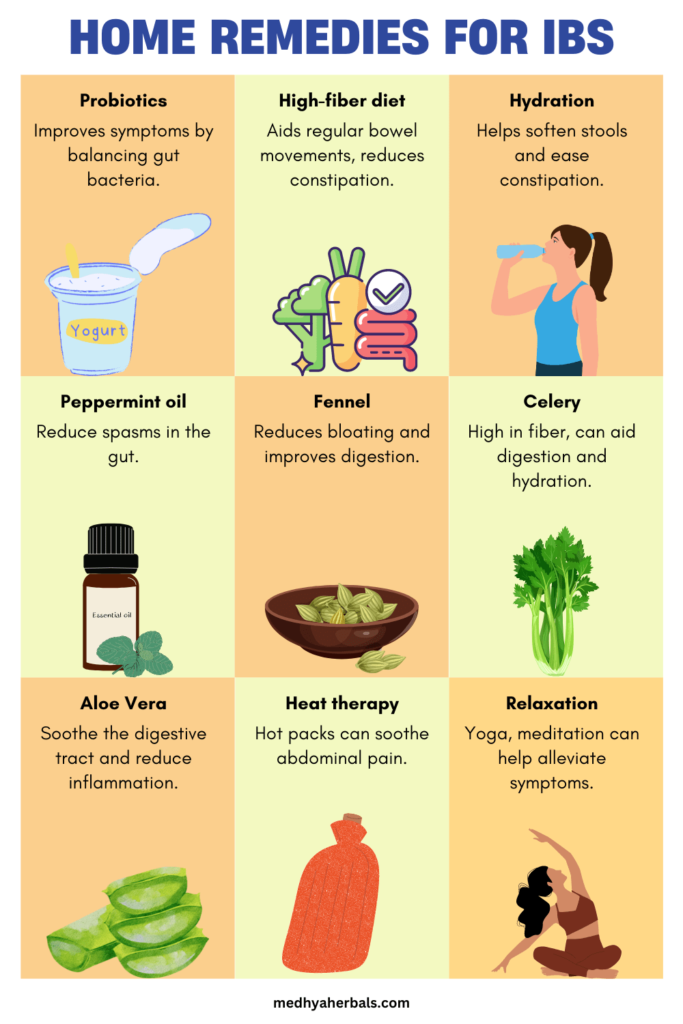
- Relaxation Techniques: Practicing deep breathing exercises, meditation, or mindfulness techniques can help reduce stress and promote relaxation, which may in turn alleviate IBS symptoms.
- Heat Therapy: Applying a heating pad or taking a warm bath can help ease abdominal pain and cramping associated with an IBS flare up.
- Gentle Exercise: Engaging in light physical activity, such as walking or gentle yoga, can help stimulate digestion and relieve constipation or bloating.
- Peppermint Oil: Peppermint oil has been found to have antispasmodic properties that can help relax the muscles of the gastrointestinal tract. Consult with your healthcare provider before using peppermint oil as a treatment option.
- Probiotics: Probiotics are beneficial bacteria that can help restore the natural balance of gut flora. They may alleviate symptoms such as bloating and improve overall gut health. Discuss with your healthcare provider before starting any probiotic supplements.
- Rest: During flare ups, it is essential to prioritize self-care and give your body the rest it needs. Rest allows your body to recover, reduces stress, and helps minimize the strain on your digestive system. Adequate sleep, taking breaks throughout the day, and engaging in relaxation techniques can all contribute to a faster recovery and symptom relief.
How to Reset the Stomach After an IBS Attack?
After an IBS flare up, it can be beneficial to reset and soothe the stomach. In fact, breaking the cycle of IBS and relaxing the gut naturally involves adopting healthy lifestyle habits. Here are some strategies to help you reset your stomach:

What to Eat after an IBS Flare Up?
While there is no one-size-fits-all approach, the following foods are generally well-tolerated by many individuals with IBS. Start with easily digestible, low-FODMAP foods, and gradually reintroduce other foods to identify triggers and assess tolerance.
- Low-FODMAP Foods: These include rice, oats, quinoa, certain vegetables (like carrots, spinach, and zucchini), lean proteins (such as chicken and fish), and some fruits (such as berries, citrus fruits, and bananas).
- Soluble Fiber: Foods rich in soluble fiber, such as oats, psyllium husk, and flaxseeds, can help regulate bowel movements and reduce constipation.
- Probiotic-Rich Foods: Probiotics can help restore gut flora balance and improve symptoms. Foods like yogurt, kefir, sauerkraut, and kimchi contain natural probiotics.
- Peppermint: Peppermint has been found to have antispasmodic properties and can help alleviate abdominal pain and cramping.
- Cooked and Easily Digestible Foods: Cooked vegetables, well-cooked grains, and lean proteins can be easier to digest and less likely to trigger symptoms.
- Herbal Teas: Peppermint tea, chamomile tea, and ginger tea can help soothe the digestive system and reduce symptoms.
- Hydration: Drink plenty of water to maintain proper hydration and support healthy digestion.
Worst Foods for IBS Flare Up Management
While individual triggers may vary, the following foods are commonly known to exacerbate IBS symptoms:
- High-FODMAP Foods: These include wheat, rye, onions, garlic, certain fruits (such as apples, pears, and watermelon), dairy products, and sugar alcohols (like sorbitol and xylitol).
- Gas-Producing Foods: Foods like beans, lentils, cabbage, broccoli, and carbonated beverages can increase bloating and gas production.
- Spicy Foods: Spicy foods can irritate the digestive system and trigger symptoms in some individuals.
- Fatty Foods: High-fat foods, such as fried foods and fatty meats, can contribute to symptoms like diarrhea and abdominal discomfort.
Warm Water
Drinking warm water has a soothing effect on the gut, thus it is really helpful for individuals undergoing IBS flare up. Warm water helps relax the muscles of the gastrointestinal tract and can promote smoother digestion. It may also provide relief from abdominal discomfort, bloating, and cramping. Sipping warm water throughout the day, especially before and after meals, can aid in digestion, promote proper bowel movement and alleviate IBS symptoms.
- Constipation Relief: Adequate hydration softens stools, making them easier to pass and reducing the risk of constipation, a common symptom of IBS.
- Promoting Regular Bowel Movements: Drinking water can help promote regular bowel movements, supporting the normal functioning of the digestive system.
Fasting
Fasting, or giving your digestive system a break from food for a specific period, can be beneficial for some individuals with IBS. It allows the gut to rest and recover. However, fasting should be approached with caution and under the guidance of a healthcare professional, especially if you have specific dietary needs or underlying health conditions. Intermittent fasting, where you limit the eating window to certain hours of the day, may be a more suitable option for some individuals.
Adequate Sleep
Getting sufficient sleep is essential for overall well-being, including gut health. Aim for 7-8 hours of quality sleep each night. Establish a bedtime routine, create a comfortable sleep environment, and prioritize sleep to support your body’s natural healing and repair processes.
Sleeping Positions
Sleeping positions can also affect IBS symptoms. Here are a few tips:
- Elevated Head: Raising the head of your bed or using an extra pillow can help alleviate symptoms of acid reflux, which may occur alongside IBS.
- Left Side Sleeping: Sleeping on your left side can aid digestion by allowing gravity to facilitate the movement of food through the digestive tract.
- Comfort and Relaxation: Find a sleeping position that is comfortable for you and promotes relaxation. A relaxed body can help reduce stress and tension in the gut, which can contribute to IBS symptoms.
Stress Management
Stress is known to worsen IBS symptoms. Managing stress effectively can have a positive impact on your gut health. Consider the following techniques to help break the IBS cycle and relax the gut naturally:
- Relaxation Techniques: Engage in activities like deep breathing exercises, meditation, yoga, or mindfulness to reduce stress levels and promote relaxation.
- Regular Exercise: Incorporate regular exercise into your routine. Physical activity can help reduce stress, improve digestion, and promote overall well-being.
Conclusion
Living with irritable bowel syndrome (IBS) and managing its flare ups can be a challenging and frustrating experience. We understand the struggles you face in finding relief from this condition. However, there is hope. By adopting the right strategies, making lifestyle adjustments, and seeking the guidance of experts, you can regain control over your gut health and experience long-lasting relief.
At Medhya Herbals, we specialize in Ayurvedic natural treatments for women’s health and wellness, including IBS management. Our Ayurvedic doctors are experienced in addressing the root causes of IBS and providing personalized treatment plans tailored to your unique needs. We empathize with your journey and are here to offer the support and guidance you need to find permanent relief from IBS.
It’s time to take that crucial step toward reclaiming your quality of life. Schedule a consultation with our Ayurvedic doctors at Medhya Herbals today. They will thoroughly assess your symptoms, triggers, and individual constitution to create a personalized treatment plan that addresses the root causes of your IBS flare ups. Our Ayurvedic approach focuses on restoring balance, nourishing your gut, and promoting overall well-being.
Don’t let IBS control your life any longer. Embrace the power of Ayurveda and discover a path to lasting relief. Schedule your consultation with Medhya Herbals now and embark on a journey toward a healthier, happier you.
FAQ
How to Identify if One is Suffering from IBS?
If you suspect that you may be suffering from IBS, it is important to consult with a healthcare professional for an accurate diagnosis. However, there are common signs and criteria used to identify IBS, including:
- Recurrent abdominal pain or discomfort at least three days per month for the last three months.
- Relief of pain or discomfort after a bowel movement.
- Changes in the frequency or consistency of bowel movements.
- The presence of other symptoms, such as bloating, gas, or mucus in the stool.
Remember, only a healthcare professional can provide a definitive diagnosis based on a thorough evaluation of your symptoms, medical history, and possibly additional tests. If you suspect you may have IBS, seek medical advice to ensure appropriate management and treatment.
Can IBS Flare Up Suddenly and Go Away on Its Own?
IBS symptoms can fluctuate over time, with periods of remission and flare ups. While it is possible for IBS symptoms to subside on their own, it is uncommon for the condition to completely resolve without intervention. IBS is a chronic condition, and effective management strategies are typically necessary to control symptoms and prevent flare ups.
Why are IBS flare ups so painful?
IBS flare ups can be painful due to the complex interaction between the gastrointestinal system and the nervous system. In individuals with IBS, the intestines may become hypersensitive and more prone to contracting forcefully or irregularly. These abnormal contractions can lead to abdominal pain and cramping. Additionally, inflammation, increased sensitivity of the nerve endings in the gut, and the release of certain substances can further contribute to the pain experienced during IBS flare ups. The exact mechanisms behind the pain in IBS are not fully understood, but it is believed to involve a combination of factors, including altered gut motility, increased gut sensitivity, and abnormal pain processing in the brain-gut axis.
Can you eat bread with IBS?
The suitability of bread for individuals with IBS can vary depending on the specific triggers and sensitivities of each person. Some types of bread, particularly those made with refined wheat flour, can be problematic for individuals with IBS due to their high FODMAP content and potential to cause bloating, gas, and digestive discomfort. However, there are alternative options available, such as gluten-free bread made from ingredients like rice, quinoa, or oats, which may be better tolerated. It is recommended to work with a healthcare professional or a registered dietitian experienced in managing IBS to determine the most appropriate bread choices based on individual sensitivities and dietary needs.
Does IBS cause smelly gas?
Yes, IBS can cause smelly gas. Individuals with IBS may experience increased gas production in the gastrointestinal tract, which can lead to the presence of foul-smelling gas. The abnormal contractions and motility issues associated with IBS can result in slower or faster movement of food through the digestive system, affecting the digestion and fermentation of certain substances. This can lead to the production of gases, such as hydrogen sulfide and methane, which can contribute to strong-smelling gas. Additionally, certain dietary triggers, such as high-FODMAP foods, can further exacerbate gas production and odor in individuals with IBS.
How do you stop an IBS attack fast?
Stopping an IBS attack quickly can be challenging as it varies from person to person. However, there are some strategies that may help alleviate symptoms. One approach is to try relaxation techniques like deep breathing, meditation, or mindfulness to reduce stress and calm the nervous system. Avoiding trigger foods and opting for a bland diet, such as easily digestible foods and low-FODMAP options, may also provide relief. Additionally, over-the-counter medications like antispasmodics or antidiarrheals may help manage specific symptoms. It’s important to consult with a healthcare professional for personalized advice and to develop a comprehensive management plan for your IBS.
References
- “The Efficacy of Ayurvedic Medicines for Irritable Bowel Syndrome: A Systematic Review and Meta-Analysis.” Evidence-Based Complementary and Alternative Medicine, Hindawi, 7 May 2021, https://www.hindawi.com/journals/ecam/2021/6623816/.
- “Ayurvedic and Conventional Treatment for Irritable Bowel Syndrome: A Randomized Double-Blind Clinical Trial.” Journal of Ayurveda and Integrative Medicine, Elsevier, 1 Jul. 2017, https://www.sciencedirect.com/science/article/pii/S0975947617300839.
- “Efficacy of Ayurvedic treatment modalities in patients with Irritable Bowel Syndrome: A randomized controlled trial.” Journal of Ayurveda and Integrative Medicine, Elsevier, 1 Oct. 2019, https://www.sciencedirect.com/science/article/pii/S0975947619301583.
- “Herbal remedies for irritable bowel syndrome: a systematic review.” Journal of Pharmacy and Pharmacology, Wiley Online Library, 10 May 2021, https://onlinelibrary.wiley.com/doi/full/10.1111/jphp.13475.
- “The effect of yoga on irritable bowel syndrome: a systematic review and meta-analysis.” Complementary Therapies in Medicine, Elsevier, 1 Oct. 2019, https://www.sciencedirect.com/science/article/pii/S0965229919302955.
- “Effect of probiotics on Irritable Bowel Syndrome: a systematic review and meta-analysis of randomized controlled trials.” Journal of Gastrointestinal and Liver Diseases, National Institute of Health, 2019, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6738735/.
- “The therapeutic effect of Aloe vera in gastrointestinal disorders: a systematic review and meta-analysis.” Journal of Research in Medical Sciences, National Institute of Health, 2019, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6843916/.
- “Fennel and its potential beneficial effects in critical health conditions.” Journal of Food and Drug Analysis, Elsevier, 2018, https://www.sciencedirect.com/science/article/pii/S1021949817301897.
- “Peppermint oil for the treatment of irritable bowel syndrome: a systematic review and meta-analysis.” Journal of Clinical Gastroenterology, National Institute of Health, 2014, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4286770/.
- “The effect of ginger in the treatment of Irritable Bowel Syndrome: a systematic review and meta-analysis.” Journal of Functional Foods, Elsevier, 1 Jan. 2021, https://www.sciencedirect.com/science/article/pii/S1756464620307185.

