As an Ayurvedic practitioner, I encounter many women seeking help for PCOS (Polycystic Ovary Syndrome) and insulin resistance, a challenging situation that significantly affects their weight and fertility. While PCOS is a common reproductive disorder in women, a large number are unaware of its strong connection with insulin resistance, a condition where the body struggles to respond effectively to the hormone insulin.
This relationship between PCOS and insulin resistance is characterized by hyperinsulinemia, a state of elevated insulin levels, which can make PCOS symptoms worse and increase the risk of developing prediabetes or type 2 diabetes.
In this comprehensive guide, I will share Ayurvedic natural solutions to address the root causes and help manage both PCOS and insulin resistance. So, let’s explore the link between PCOS and insulin resistance so that you have the much needed knowledge to find relief from the conditions.
Understanding the Link Between PCOS and Insulin Resistance
PCOS, or Polycystic Ovary Syndrome, is a prevalent hormonal disorder among women of reproductive age, characterized by irregular menstrual cycles, excess androgens production, and polycystic ovaries. Insulin resistance, on the other hand, occurs when the body’s cells do not respond effectively to insulin, the hormone responsible for regulating blood sugar levels. The connection between PCOS and insulin resistance is intricate and multifaceted, with several factors contributing to the development and progression of both conditions.
Hormonal Imbalance
A primary contributor to the link between PCOS and insulin resistance is hormonal imbalance. Women with PCOS often have elevated levels of insulin due to decreased insulin sensitivity. This state, known as hyperinsulinemia, may stimulate the ovaries to produce excessive amounts of androgens, such as testosterone. High androgen levels can further disrupt the menstrual cycle, leading to anovulation and exacerbating PCOS symptoms.
Obesity
Excessive weight gain is a common risk factor for both PCOS and insulin resistance. Excess body weight, particularly around the abdomen, can contribute to insulin resistance by impairing the body’s ability to use insulin effectively. Moreover, obesity can worsen hormonal imbalances in women with PCOS, leading to more severe symptoms and increased insulin resistance.
Inflammation
Chronic inflammation has been linked to both PCOS and insulin resistance. Inflammation can interfere with insulin signaling pathways, impairing the body’s ability to respond to insulin effectively. Moreover, PCOS is associated with elevated levels of inflammatory markers, which may contribute to the development of insulin resistance.
Genetic Factors
Genetic predisposition may play a role in the development of both PCOS and insulin resistance. Research has identified several genes associated with insulin resistance and PCOS, suggesting that women with a family history of these conditions may have an increased risk of developing both.
Compounding Effects
The presence of insulin resistance in women with PCOS can create a vicious cycle. As insulin resistance worsens, it can lead to higher insulin levels, which in turn can exacerbate PCOS symptoms by increasing androgen production and inflammation. This cycle perpetuates itself, leading to the progression of both conditions and increasing the risk of developing long-term health complications such as type 2 diabetes and cardiovascular disease.
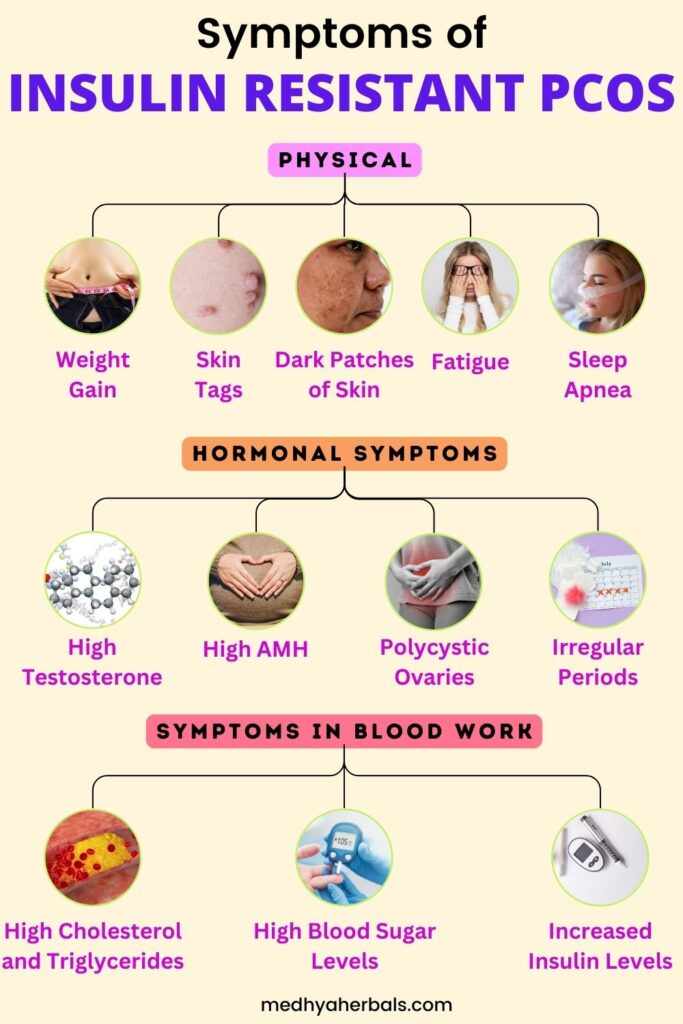
Identifying Signs of Insulin Resistance in Women with PCOS
Recognizing the signs of insulin resistance in women with PCOS is essential for early diagnosis and intervention. Insulin resistance can exacerbate PCOS symptoms and increase the risk of long-term health complications. The following sections outline some key indicators of insulin resistance in women with PCOS.
Physical Symptoms
Weight Gain and Difficulty Losing Weight
Insulin resistance can lead to weight gain, particularly around the abdomen. Women with PCOS and insulin resistance may find it challenging to lose weight, even with diet and exercise.
Dark Patches of Skin
Acanthosis nigricans, characterized by dark, velvety patches of skin, often appear in areas where skin folds, such as the neck, armpits, and groin. This skin condition can be a sign of insulin resistance.
Skin Tags
Small, flesh-colored growths known as skin tags are common in people with insulin resistance. They usually appear in areas where skin rubs together, such as the neck, armpits, or under the breasts.
Metabolic and Hormonal Symptoms
Irregular Menstrual Cycles
Insulin resistance can exacerbate hormonal imbalances in women with PCOS, leading to irregular or absent menstrual cycles.
Polycystic Ovaries
Women with PCOS and insulin resistance may have enlarged ovaries with multiple small cysts, visible through ultrasound examination.
Elevated Androgen Levels
Insulin resistance can stimulate the production of excess androgens, such as testosterone, worsening PCOS symptoms and contributing to issues like hirsutism (excess facial and body hair), acne, and male-pattern baldness.
Blood Test Results
High Fasting Blood Sugar Levels
Elevated fasting blood sugar levels can indicate insulin resistance, as the body struggles to regulate glucose effectively.
Elevated Insulin Levels
High insulin levels, or hyperinsulinemia, can be a sign of insulin resistance, as the body produces more insulin in an attempt to overcome the decreased sensitivity of cells to insulin.
Abnormal Lipid Profile
Insulin resistance can lead to an abnormal lipid profile, characterized by high triglycerides, low high-density lipoprotein (HDL) cholesterol, and high low-density lipoprotein (LDL) cholesterol.
By identifying these signs of insulin resistance in women with PCOS, your doctor can develop targeted treatment plans to address both conditions.
Decoding the PCOS Belly
The term “PCOS belly” refers to the stubborn abdominal fat often associated with Polycystic Ovary Syndrome. One of the main reasons for the PCOS belly is insulin resistance. As the body becomes less responsive to insulin, it produces more of the hormone, leading to weight gain, particularly around the abdomen.
In addition, hormonal imbalances in PCOS, including high testosterone levels can cause weight gain and fat distribution patterns similar to those observed in men, including an increased tendency to accumulate abdominal fat.
High abdominal fat in PCOS may also result from chronic inflammation, which is common in women with PCOS. It can contribute to the development of the PCOS belly by impairing the body’s ability to burn fat, thus promoting fat storage, particularly in the abdominal area.
Ayurvedic Treatment for PCOS and Insulin Resistance
PCOS and Insulin Resistance are considered to be Tridoshic imbalance involving vata, pitta and kapha dosha. There is also high levels of toxin build up known as “Ama”, a thick and gooey substance that blocks the reproductive channels, thus causing irregular ovulation and blocked fallopian tubes in some cases. Ama also triggers inflammation and hampers fat metabolism in the body, causing excessive weight gain in PCOS and insulin resistance.
Thus, Ayurvedic natural treatment for insulin resistance pcos involves detoxification and hormone balance to support fertility and proper metabolism in women with PCOS. In addition, dietary changes and lifestyle adaptations involving regular yoga, massage therapy and herbal supplements help with proper treatment.
Ayurvedic Herbs and Medicines for Insulin Resistance and PCOS

Ayurvedic herbs and medicines are highly effective to address insulin resistance and promote hormonal balance. These herbs work to balance the body’s energies (doshas), flush the toxins out and promote regular ovulation in PCOS. It’s important to consult with an Ayurvedic practitioner or healthcare professional before starting any herbal treatments to ensure they are suitable for your individual needs.
Cinnamon (Cinnamomum zeylanicum)
Cinnamon is a common spice known for its blood sugar-lowering properties. It can improve insulin sensitivity and help regulate blood sugar levels. Add cinnamon to your meals, smoothies, sweet porridge or herbal teas.
Fenugreek (Trigonella foenum-graecum)
Fenugreek seeds have been shown to lower blood sugar levels and improve insulin sensitivity. They also possess antioxidant and anti-inflammatory properties, which can benefit women with PCOS.
Amla (Emblica officinalis)
Amla, also known as Indian gooseberry, is a rich source of antioxidants and Vitamin C. It can help regulate blood sugar levels, support hormonal balance, and reduce inflammation. Amla can be consumed as a powder, juice, or in supplement form.
Ashwagandha (Withania somnifera)
Ashwagandha is an adaptogenic herb known for its ability to help the body cope with stress. It can support hormonal balance, regulate blood sugar levels, and improve insulin sensitivity.
Shatavari (Asparagus racemosus)
Shatavari is a popular herb in Ayurvedic medicine for promoting female reproductive health. It can help balance hormones, reduce inflammation, and support overall well-being in women with PCOS.
Licorice (Glycyrrhiza glabra)
Licorice root has been shown to reduce testosterone levels in women with PCOS, which can help alleviate symptoms such as hirsutism and acne. It also possesses anti-inflammatory properties.
Turmeric (Curcuma longa)
Turmeric, containing the active compound curcumin, is known for its anti-inflammatory and antioxidant properties. It can help reduce inflammation and improve insulin sensitivity in individuals with insulin resistance and PCOS.
Best Diet for Insulin Resistance and PCOS
A well-planned diet can be an effective tool for managing insulin resistance and PCOS symptoms. The following dietary recommendations can help improve insulin sensitivity, balance hormones, and promote overall health in women with insulin-resistant PCOS.

Low-Glycemic-Index (GI) Foods
Foods with a low glycemic index release glucose slowly into the bloodstream, helping maintain stable blood sugar levels and reducing insulin spikes. Incorporate low-GI foods, such as:
- Non-starchy vegetables (leafy greens, broccoli, cauliflower)
- Whole grains (oats, barley, quinoa)
- Legumes (lentils, chickpeas, black beans)
- Nuts and seeds (almonds, walnuts, chia seeds)
Lean Proteins
Lean protein sources can help regulate blood sugar levels and promote satiety. Include:
- Poultry (chicken, turkey)
- Fish (salmon, tuna, sardines)
- Plant-based proteins (tofu, tempeh, edamame)
Healthy Fats
Incorporate healthy fats, which can help improve insulin sensitivity and reduce inflammation:
- Avocado
- Olive oil
- Nuts and seeds
- Fatty fish (salmon, mackerel, sardines)
High-Fiber Foods
Fiber can slow down the absorption of sugar in the bloodstream, helping manage blood sugar levels and insulin response. Aim for a variety of high-fiber foods:
- Fruits (berries, apples, pears)
- Vegetables (broccoli, Brussels sprouts, artichokes)
- Whole grains (brown rice, whole wheat pasta, quinoa)
- Legumes (beans, lentils, chickpeas)
Antioxidant-Rich Foods
Antioxidant-rich foods can help combat inflammation and oxidative stress, both of which are common in women with PCOS. Include:
- Fruits (berries, cherries, grapes)
- Vegetables (kale, spinach, red cabbage)
- Nuts (walnuts, pecans, almonds)
- Spices (turmeric, cinnamon, ginger)
Foods to Avoid
Certain foods can worsen insulin resistance and PCOS symptoms. Limit or avoid:
- Refined carbohydrates (white bread, white rice, pastries)
- Sugary beverages (soda, fruit juices)
- Processed foods (chips, cookies, frozen meals)
- Trans fats and excessive saturated fats (fried foods, fatty meats)
Pay attention to portion sizes and ensure meals are balanced, including a mix of low-GI carbohydrates, lean proteins, and healthy fats. This will help maintain stable blood sugar levels and promote satiety, reducing the risk of overeating and weight gain.
Lifestyle Changes for Managing Insulin Resistance
In addition to dietary modifications, implementing certain lifestyle changes can significantly improve insulin sensitivity and help manage insulin resistance. Here are highly effective tips for weight loss and hormonal balance in PCOS and insulin resistance.
Regular Exercise
Physical activity plays a crucial role in managing insulin resistance. Engaging in regular exercise can improve insulin sensitivity and support weight loss. Consider incorporating the following types of exercise into your routine:
Aerobic Exercise
Aerobic activities, such as walking, jogging, swimming, or cycling, can help lower blood sugar levels, improve insulin sensitivity, and support cardiovascular health. Aim for at least 150 minutes of moderate-intensity aerobic exercise per week, divided into several sessions.
Resistance Training
Strength training exercises, such as weight lifting or bodyweight exercises, can help build muscle mass, boost metabolism, and enhance insulin sensitivity. Aim for two to three sessions of resistance training per week, targeting all major muscle groups.
High-Intensity Interval Training (HIIT)
HIIT involves alternating between short bursts of intense exercise and recovery periods. This type of training can improve insulin sensitivity and promote fat burning. Incorporate one to two HIIT sessions per week, adjusting the intensity and duration according to your fitness level.
Weight Loss Tips
Losing even a modest amount of weight can have a significant impact on insulin sensitivity. Consider the following tips to support healthy weight loss:
Set Realistic Goals
Establish achievable weight loss goals to maintain motivation and track progress. Aim for a gradual, sustainable weight loss rate of 0.5 to 1 kilogram (1 to 2 pounds) per week.
Monitor Food Intake
Keep a food diary or use a smartphone app to track daily food consumption. Monitoring food intake can help identify patterns, portion sizes, and areas for improvement.
Establish a Support System
Share your weight loss goals with friends, family, or a support group. Having a network of people who understand and encourage your efforts can help keep you motivated and accountable.
Prioritize Sleep
Getting enough quality sleep is essential for weight loss and overall health. Aim for seven to nine hours of sleep per night and establish a regular sleep schedule.
Manage Stress
Chronic stress can contribute to weight gain and make it more challenging to lose weight. Incorporate stress-management techniques, such as meditation, deep breathing exercises, or yoga, to help control stress levels.
Conclusion
As we reach the end of our journey, it’s crucial to remember that understanding and managing PCOS and insulin resistance is an ongoing process. With the right information and support, you can take charge of your health and improve your quality of life.
Don’t delay seeking treatment for PCOS and insulin resistance! Timely intervention can prevent long-term health complications and improve your quality of life. At Medhya Herbals, our highly experienced Ayurvedic doctors can help you find relief from your symptoms. We offer personalized treatment plans tailored to your individual needs, using a holistic approach that combines the wisdom of Ayurveda with modern medical knowledge.
Begin your healing journey and get in touch with Medhya Herbals today. Together, we can develop a comprehensive treatment plan to help you manage PCOS and insulin resistance for sustained relief.
References
- Polycystic ovary syndrome (PCOS) – The National Institute of Child Health and Human Development, 2021.
- Insulin Resistance & Prediabetes – American Diabetes Association, 2018.
- The relationship between polycystic ovary syndrome and insulin resistance – Current Pharmaceutical Design, 2013.
- Insulin resistance in polycystic ovary syndrome: A systematic review and meta-analysis of euglycaemic-hyperinsulinaemic clamp studies – Human Reproduction Update, 2016.
- Lifestyle changes in women with polycystic ovary syndrome – Cochrane Database of Systematic Reviews, 2011.
- The effect of a low-carbohydrate, ketogenic diet versus a low-glycemic index diet on glycemic control in type 2 diabetes mellitus – Nutrition & Metabolism, 2008.
- Dietary composition in the treatment of polycystic ovary syndrome: A systematic review to inform evidence-based guidelines – Journal of Clinical Endocrinology & Metabolism, 2013.
- Effects of exercise on insulin resistance in women with polycystic ovary syndrome – Iranian Journal of Reproductive Medicine, 2011.
- Adrenal androgen excess and body mass index in polycystic ovary syndrome – Journal of Clinical Endocrinology & Metabolism, 2006.
- Polycystic ovary syndrome and insulin: Our understanding in the past, present and future – Women’s Health, 2015.

